Developing a medical app in the U.S. means navigating strict regulations to protect sensitive health data and ensure compliance. Key laws like HIPAA, the FTC Act, and the FD&C Act govern how apps handle Protected Health Information (PHI). Non-compliance can lead to severe penalties, with HIPAA fines reaching up to $50,000 per incident.
Here’s what you need to know:
- HIPAA Compliance: Apps managing PHI must follow rules for privacy, security, and breach notifications. Encryption, multi-factor authentication, and risk assessments are essential safeguards.
- Additional Regulations: Depending on the app's purpose, laws like the 21st Century Cures Act, COPPA, and state-specific laws like the CCPA may apply.
- FDA Oversight: Apps functioning as medical devices must meet FDA requirements for safety and effectiveness.
- Security Measures: Use encryption, access controls, and regular audits to protect health data.
- Adalo for Development: Platforms like Adalo streamline app creation and deployment across web, iOS, and Android without rebuilding for each platform, while supporting HIPAA compliance.
Compliance is not a one-time task - it requires continuous updates, audits, and adherence to evolving regulations. Tools like the “Mobile Health Apps Interactive Tool” and HHS Security Risk Assessment Tool can help you stay on track.
Mastering HIPAA Compliance in Healthcare Apps: Top 5 Developer Questions Answered
Regulatory Requirements for Medical Apps in the U.S.

Key U.S. Regulations for Medical Apps: Oversight Bodies and Focus Areas
If you're developing a medical app, the first question to tackle is: does your app deal with Protected Health Information (PHI)? PHI refers to identifiable health data like names, Social Security numbers, or birth dates. When this data is stored or transmitted electronically, it becomes electronic PHI (ePHI), triggering specific regulations you must follow.
But HIPAA isn’t the only regulation you need to consider. Depending on your app’s purpose, it might also fall under other federal laws, such as the Federal Food, Drug, and Cosmetic Act (FD&C Act) or the FTC Act, as well as state laws like the California Consumer Privacy Act (CCPA). Here’s a quick look at key federal regulations that could impact your app:
| Regulation | Oversight Body | Focus Area |
|---|---|---|
| FD&C Act | FDA | Ensures safety and effectiveness for apps functioning as medical devices |
| FTC Act | FTC | Protects against deceptive marketing and unfair privacy practices |
| Health Breach Notification Rule | FTC | Requires notification of data breaches for apps not covered by HIPAA |
| 21st Century Cures Act | ASTP/ONC/OIG | Prevents information blocking and promotes interoperability |
| COPPA | FTC | Safeguards privacy for children under 13 |
The stakes are high. Since 2016, HIPAA-related fines have exceeded $40 million, with penalties ranging from $100 to $50,000 per incident, depending on the level of negligence. Medical data is a prime target for cybercriminals, reportedly selling for three times the value of financial data on the black market. With this in mind, understanding these regulations is crucial before diving into HIPAA’s specific requirements.
What You Need to Know About HIPAA Compliance
HIPAA (the Health Insurance Portability and Accountability Act of 1996) establishes national standards to protect patient data. It’s built around four main rules:
- Privacy Rule: Dictates when PHI can be used or disclosed.
- Security Rule: Requires physical, administrative, and technical safeguards for ePHI.
- Breach Notification Rule: Mandates notifying the Department of Health and Human Services (HHS) and affected individuals in case of a data breach.
- Omnibus Rule: Extends HIPAA compliance to business associates.
If your app creates, receives, maintains, or transmits PHI on behalf of a covered entity (like a hospital or health plan), you’re considered a "business associate" under HIPAA. As the Office for Civil Rights (OCR) explains:
"A business associate relationship exists if an entity creates, receives, maintains, or transmits ePHI on behalf of a covered entity (directly or through another business associate) to carry out the covered functions of the covered entity."
Before handling PHI, you must sign a Business Associate Agreement (BAA) with the covered entity. Ignoring this can lead to hefty fines. For instance, in 2017, Presence Health paid $475,000 for failing to report a data breach on time, and Mount Sinai-St. Luke's Hospital faced a $387,000 fine after an HIV clinic improperly disclosed a patient’s PHI.
The Security Rule, finalized in 2003, requires you to document your HIPAA policies and assessments for at least six years. Your app should also adhere to the "minimum necessary" standard, ensuring it only accesses or transmits the smallest amount of PHI needed for a given task. While encryption isn’t always mandatory, failing to encrypt devices handling PHI is a common cause of HIPAA violations.
When HIPAA Applies to Your App
HIPAA applies if your app processes PHI "on behalf of" a covered entity. For example, if a hospital hires you to build a telemedicine platform for its doctors, your app must comply with HIPAA. However, if a user downloads a fitness tracker for personal use and the app doesn’t connect to a healthcare provider, HIPAA typically doesn’t apply.
This distinction is critical, as the OCR clarifies:
"Once health information is received from a covered entity, at the individual's direction, by an app that is neither a covered entity nor a business associate under HIPAA, the information is no longer subject to the protections of the HIPAA Rules."
Apps subject to HIPAA often include telemedicine platforms, electronic health record systems, appointment schedulers integrated with hospital systems, and prescription management tools. On the flip side, fitness trackers, nutrition apps, meditation tools, and symptom checkers that don’t share data with healthcare providers usually fall outside HIPAA’s scope.
For guidance, you can use the Mobile Health Apps Interactive Tool created by the FTC, OCR, ONC, and FDA. This tool helps you determine your compliance obligations based on your app’s features and data handling.
Other U.S. Regulations That May Apply
HIPAA isn’t the only regulation shaping compliance for medical apps. The FDA oversees software that qualifies as a "medical device" under the FD&C Act, which includes apps designed to diagnose, treat, or prevent diseases. As the FDA notes:
"The FDA's policies are independent of the platform on which they might run, are function-specific, and apply across platforms."
Since March 2023, premarket submissions for cyber devices must include postmarket vulnerability plans and a Software Bill of Materials (SBOM).
The FTC’s Health Breach Notification Rule applies to health apps not covered by HIPAA. According to the FTC:
"The FTC's Health Breach Notification Rule applies to most health apps that aren't covered by HIPAA because most developers of health apps are acting as 'health care providers' by furnishing health care services or supplies – in this case, apps – to consumers."
If a data breach occurs, you’re required to notify consumers, the FTC, and in some cases, the media. Additionally, misleading practices - like sharing health data with third parties after promising privacy - can result in enforcement actions under the FTC Act.
Other regulations to consider include:
- COPPA: Protects privacy for children under 13.
- 21st Century Cures Act: Prohibits practices that block access to electronic health information.
- Opioid Addiction Recovery Fraud Prevention Act (OARFPA): Penalizes deceptive practices related to substance use disorder treatments.
- State Laws: For example, California’s CCPA imposes additional privacy requirements.
It’s also a good idea to use just-in-time notices to inform users about sensitive data collection - like geolocation - both during installation and when data collection begins.
Security and Privacy Features for Medical Apps
To safeguard electronic protected health information (ePHI), it’s crucial to implement a combination of technical, administrative, and physical safeguards. These measures align with the HIPAA Security Rule, which outlines the necessary steps for compliance. These include encryption, access controls, risk analyses, workforce training, and managing access to devices and facilities. As the U.S. Department of Health and Human Services explains:
"The Security Rule is designed to be flexible, scalable, and technology neutral, enabling a regulated entity to implement policies, procedures, and technologies that are appropriate for the entity's particular size, organizational structure, and risks to ePHI."
This flexibility allows you to tailor your app's security measures to its unique requirements, but certain baseline features are non-negotiable.
Core Security Features to Include
Start by encrypting data both at rest and in transit using strong protocols like NIST SP 800-52 for TLS and FIPS 140-2 for cryptography. The Federal Trade Commission (FTC) underscores the importance of robust encryption:
"Encryption is a key security protection for the health information your app collects. Select stronger encryption methods over weaker ones."
Other essential features include:
- Multi-factor authentication (MFA): This requires users to confirm their identity using a combination of a password and a secondary code sent via email or text.
- Automatic log-off: To prevent unauthorized access when devices are left unattended.
- Password security: Store passwords in a salted, hashed format to enhance protection.
- Role-based access controls: Limit permissions to only what’s necessary for specific roles, adhering to the principle of least privilege. For instance, if your app only requires geolocation data, avoid requesting access to contacts or photos.
- Audit controls: Monitor and document system activity to detect anomalies.
- Integrity controls: Ensure data remains unaltered unless authorized.
- Rate limiting: Protect against brute force attacks by restricting the number of login attempts.
Additionally, enforce strict policies for handling hardware that processes ePHI to prevent unauthorized access or data breaches.
Working with HL7 and FHIR Standards
To ensure secure data sharing, adopt HL7 (Health Level Seven) and FHIR (Fast Healthcare Interoperability Resources) standards. These protocols enable seamless interoperability across systems while adhering to HIPAA's “minimum necessary” requirement. Even when using standardized APIs, you are responsible for securing any data your app processes. Carefully vet third-party SDKs or libraries to avoid vulnerabilities or unnecessary permissions.
Risk Assessments and Vulnerability Testing
Performing regular risk assessments is critical to identifying and addressing potential threats. This process should occur at least annually or whenever new technologies or operations are introduced. The Office for Civil Rights highlights the importance of this practice:
"Risk analysis is the first step in an organization's Security Rule compliance efforts. Risk analysis is an ongoing process that should provide the organization with a detailed understanding of the risks to the confidentiality, integrity, and availability of e-PHI."
Use tools like the HHS Security Risk Assessment (SRA) Tool or follow NIST Special Publication 800-30 for guidance. Your evaluation should cover all ePHI your app interacts with, whether stored on cloud servers, mobile devices, or local databases.
When testing for vulnerabilities, simulate real-world scenarios to uncover potential weaknesses, such as back doors or logic flaws. Focus on addressing the OWASP Top 10 most critical web application security risks and the SANS Top 25 Most Dangerous Software Errors. Stay informed about emerging threats by monitoring resources like the National Vulnerability Database.
Finally, document all security policies and assessments thoroughly. HIPAA requires these records to be retained for at least six years from their creation or last effective date. Under the HITECH Amendment, maintaining "recognized security practices" over the past 12 months may also factor into enforcement or audits by HHS.
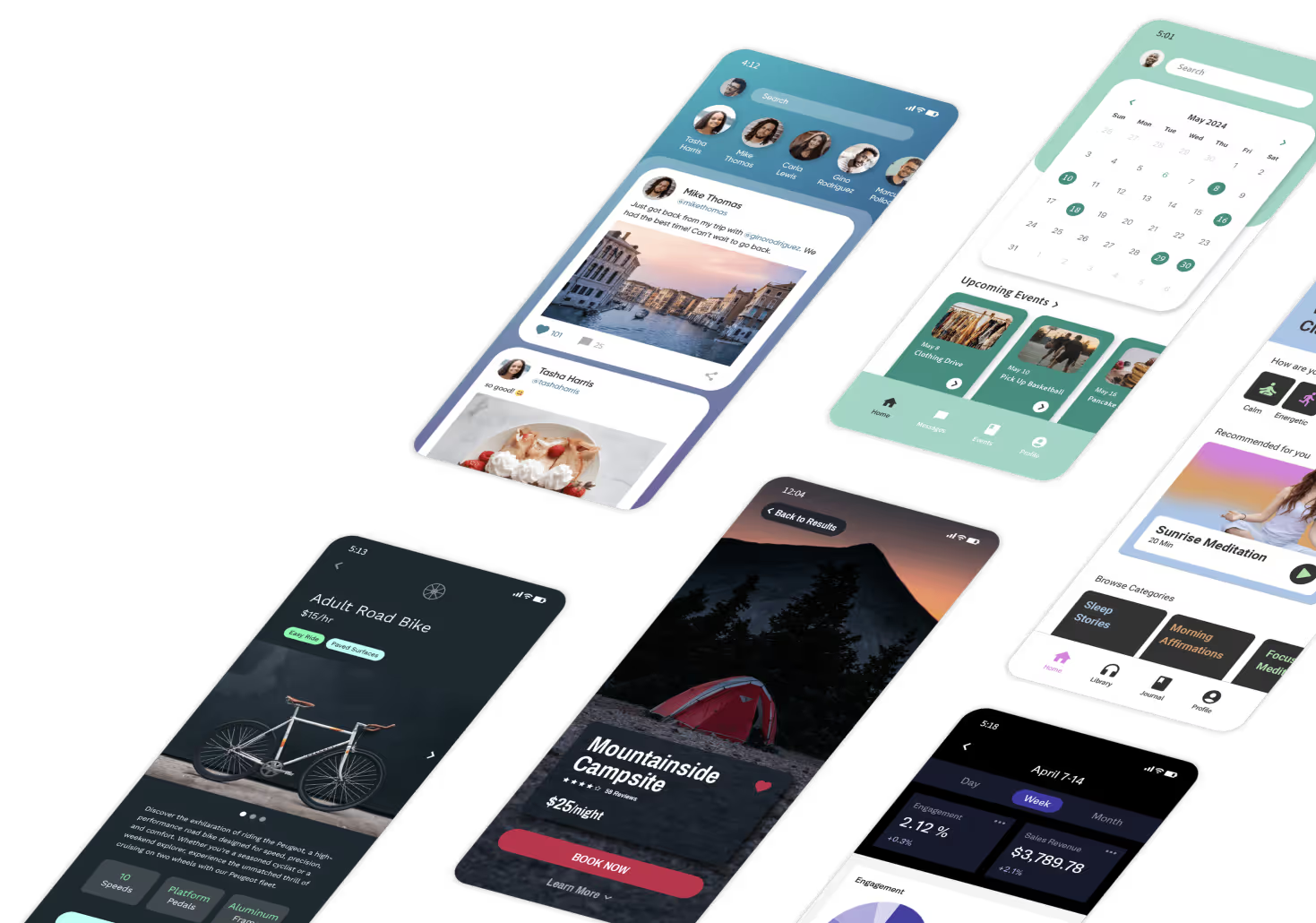
With comprehensive risk assessments and testing in place, you can confidently move forward with development. Platforms like Adalo make it easier to deploy your app as a Progressive Web App (PWA) or natively on iOS and Android, streamlining the production process while adhering to these critical security frameworks.
sbb-itb-d4116c7
Building Medical Apps with Adalo
When creating medical apps, choosing the right development platform is just as important as ensuring compliance with security standards. Adalo simplifies this process with its visual builder and hosted backend, allowing you to develop a single app that works seamlessly across web, iOS, and Android. Let’s explore how Adalo’s features, multi-platform publishing capabilities, and HIPAA compliance support make it a strong choice for medical app development.
Key Adalo Features for Medical App Development
Adalo’s visual interface makes it possible to build apps without writing code, while still meeting the strict safeguards required by HIPAA. It offers built-in user authentication, role-based access controls, and audit logging - key features for protecting electronic protected health information (ePHI). Its hosted database ensures secure data storage, and its integration with DreamFactory enables connections to legacy systems like MS SQL Server or PostgreSQL. This makes it easier to access patient data from electronic health record systems or other sources that don’t have RESTful APIs.
The platform also uses AI to assist with app generation, automatically organizing your database and layouts to speed up the development of a minimum viable product. From there, you can use the drag-and-drop editor to add features like appointment scheduling, telemedicine video calls, or secure messaging.
Publishing to Multiple Platforms from One Build
Adalo not only simplifies app development but also makes deployment across platforms effortless. With its single-codebase approach, you can build your app once and publish it on the web, iOS App Store, and Google Play Store. This eliminates the need to maintain separate native codebases for each platform, saving significant time and effort. Any updates you make in Adalo’s visual builder - whether they’re security patches, new features, or compliance adjustments - are applied across all platforms instantly, ensuring consistency and reliability.
How Adalo Supports HIPAA Compliance
If your app handles protected health information (PHI) for a hospital, clinic, or health plan, Adalo qualifies as a Business Associate under HIPAA regulations. Before launching, you’ll need to establish a Business Associate Agreement (BAA) with Adalo. The platform’s infrastructure is designed to meet the technical safeguards outlined in the HIPAA Security Rule, including encryption for data transmission, access controls, integrity checks, and audit capabilities. Adalo’s hosted backend ensures these safeguards are in place across all deployment platforms, easing the technical burden on your team.
Maintaining Compliance After Launch
Getting your medical app off the ground is just the beginning. Staying compliant is an ongoing process that requires adapting to evolving regulations and addressing new security challenges.
Staying Current with Regulatory Changes
Your medical app may fall under several federal laws, including HIPAA, the FTC Act, the FD&C Act, and the 21st Century Cures Act. To help navigate these, the HHS Office for Civil Rights (OCR) publishes a quarterly Cybersecurity Newsletter, which offers insights into emerging threats and practical advice, such as system hardening and countering social engineering attacks. Subscribing to OCR updates can provide you with timely FAQs, guidance, and technical assistance.
It’s also worth noting that OCR, by statute, considers whether a regulated entity has followed "recognized security practices" over the previous 12 months when conducting audits or enforcing the Security Rule. Incorporating these updates into your risk analysis procedures can help ensure your app stays compliant.
Regular Audits and Security Updates
HIPAA requires regular security audits to assess whether your policies and procedures align with Security Rule standards. These audits and updates should continue throughout your app’s lifecycle, even after launch. The Federal Trade Commission emphasizes the importance of this:
"New vulnerabilities arise regularly, so it's important that you have a plan for how you'll provide updates for products and how you'll communicate with consumers – even after you release your app."
To stay ahead, frequently check the National Vulnerability Database for known software issues, and establish a monitored channel where security researchers and users can report vulnerabilities. Pay close attention to third-party libraries or code integrated into your app, as these can introduce risks. Additionally, maintain all HIPAA-related documentation - including audit records and corrective actions - for at least six years to support compliance during reviews.
Tools for Compliance Management
Once your security measures are updated, specific tools can help manage compliance more efficiently. The Mobile Health Apps Interactive Tool, created by the FTC, OCR, ONC, and FDA, can guide you in identifying which federal laws apply based on your app’s functionality and data practices. For conducting routine risk analyses, the HHS Security Risk Assessment Tool and the NIST HIPAA Security Rule Toolkit are invaluable resources. Additionally, the FDA’s Digital Health Policy Navigator can clarify whether your app’s software functions fall under FDA regulation.
Platforms like Adalo simplify compliance maintenance by offering integrated deployment options. You can launch your app as a Progressive Web App (PWA) or as native apps on iOS and Android without needing to rebuild - ensuring a smooth, production-ready rollout.
Conclusion
Developing a medical app in the U.S. comes with its fair share of challenges, especially when it comes to compliance and security. Navigating regulations like HIPAA, FTC guidelines, and sometimes FDA requirements depends on how your app handles Protected Health Information (PHI). As the Office for Civil Rights puts it:
"Building privacy and security protections into technology products enhances their value by providing some assurance to users that the information is secure and will be used and disclosed only as approved or expected."
Compliance isn’t a one-and-done task - it’s an ongoing process. From day one, you’ll need to implement administrative, physical, and technical safeguards, and keep them up to date through regular risk assessments, audits, and updates. Make sure to retain HIPAA documentation for at least six years and stay ahead of evolving security threats.
To streamline the compliance process, tools like the Mobile Health Apps Interactive Tool and the HHS Security Risk Assessment and NIST HIPAA Security Rule Toolkits can be invaluable. With nearly 79% of Americans expressing concerns about how companies handle their health data, focusing on security and transparency isn’t just a regulatory necessity - it’s key to building trust with your users.
Platforms like Adalo can simplify the technical side of app development. With Adalo, you can create production-ready medical apps that work as Progressive Web Apps or native apps for iOS and Android, all from a single build.
FAQs
What regulations should I follow when developing a medical app in the U.S.?
When building a medical app in the U.S., following HIPAA (Health Insurance Portability and Accountability Act) regulations is non-negotiable. HIPAA establishes strict rules to safeguard patients' health information (PHI), focusing on privacy, security, and breach notification standards. This means developers need to implement robust measures to protect electronic PHI (ePHI) and have clear procedures in place to handle data breaches.
The HITECH Act further reinforces HIPAA by imposing higher penalties for violations and mandating quicker breach notifications. On top of that, developers should consider FTC guidelines, which stress the importance of securing user data, limiting unnecessary data collection, and maintaining clear, transparent privacy policies. Together, these regulations provide the framework for creating a medical app that is both legally compliant and ethically sound in the United States.
What do developers need to know about HIPAA when creating a medical app?
When creating a medical app in the U.S., ensuring HIPAA compliance is a must if your app deals with protected health information (PHI). This means your app needs to follow HIPAA's Privacy, Security, and Breach Notification Rules. These rules focus on safeguarding electronic PHI, restricting its use and sharing, and protecting patient rights.
If your app serves covered entities (like healthcare providers) or functions as a business associate, you're legally obligated to integrate these protections into your app's design and functionality. This involves implementing secure data storage, encryption, and strict access controls to keep sensitive information safe. Non-compliance can lead to serious legal and financial consequences, making it critical to fully understand and meet these requirements.
What are the key security measures for protecting health data in a medical app?
To safeguard health data within a medical app, it's essential to adopt a multi-layered strategy that aligns with HIPAA regulations and puts user privacy front and center. Here's how you can address this:
Administrative safeguards involve setting up a strong foundation for security. This includes conducting regular risk assessments to identify vulnerabilities, developing clear and enforceable security policies, and ensuring your team is well-trained in handling electronic protected health information (ePHI) responsibly.
Physical safeguards focus on controlling access to hardware and facilities. This might mean securing server rooms, limiting workstation usage to authorized personnel, and encrypting mobile devices while enabling remote wipe capabilities to protect data if a device is lost or stolen.
Technical safeguards are critical for securing the app itself. Employ strong password policies, enforce multifactor authentication, and encrypt data both when stored and during transmission. Features like automatic session timeouts, audit logging to monitor access, and regular vulnerability scans and updates are key to maintaining security. Collect only the data you truly need, restrict access permissions to the minimum required, and design secure authentication processes to further reduce risks.
Lastly, having a well-prepared incident response plan is non-negotiable. This plan should include steps to quickly detect breaches, notify affected individuals, and take immediate corrective action to mitigate any damage.
Related Blog Posts